Welcome to St. Paul's Senior Services
Senior Living Communities and Programs for Every Lifestyle in San Diego
St. Paul’s Senior Services has been caring for San Diego seniors since 1960. With the changing needs of today’s older adults, our services have expanded to bring innovative choices to seniors and caregivers seeking resources for independent living, assisted living and personal care, memory care, medical oversight, and life enrichment.
Located throughout San Diego, St. Paul’s provides affordable senior living communities, innovative services, and comprehensive programs in a non-denominational environment with great value placed on optimal independence at all stages of life. Our history of innovation has been guided by our overall mission and vision. We would love to give you a tour of any of our communities or programs. Call 1-833-ST PAULS to speak with our friendly staff. We look forward to assisting you.
Senior Living Services for San Diegans

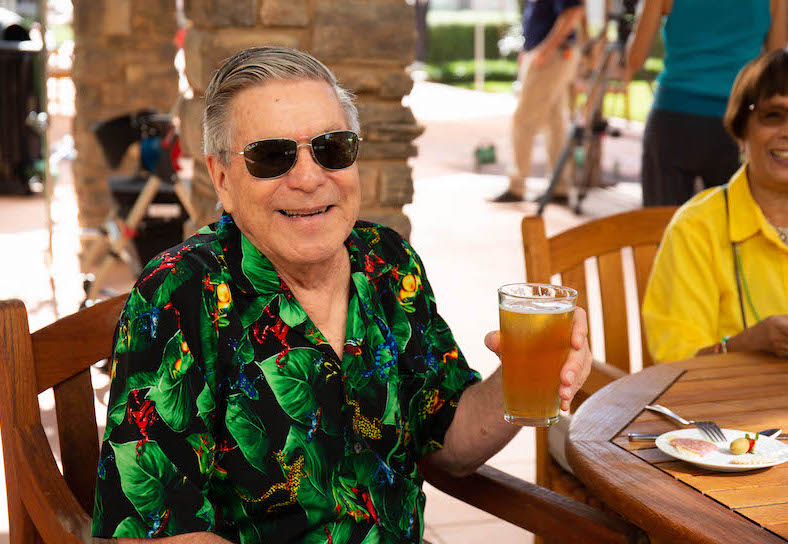
Independent Living
Independent senior living, also known as active retirement living, is for seniors 55 years and older with no need for care services. Active retirement living is a great option for seniors who wish to form new relationships in a thriving community, maintain their independence without the upkeep of a home, and experience an array of purposeful activities and programs.
Assisted Living
For seniors requiring senior care services including medication management, bathing, grooming, and assistance with activities of daily living. St. Paul’s certified caregivers are trained to ensure residents receive excellent care in a compassionate setting. Assisted living is appropriate for older adults that need some supervision and care, but not at the level of a skilled nursing facility.

Memory Care
An age-in-place community makes it easy for seniors to transition from independent living to assisted living without needing to move. At St. Paul’s, our age-in-place community allows residents to stay in their same room even when more care is required. Each resident is routinely assessed to make sure they are receiving the proper level of care as their needs increase.

Respite Care
Short Term Stays
For seniors who live in their own homes and are being cared for by a family member or friend, St. Paul’s offers short-term respite care (stays) at our communities. This allows family caregivers the time for respite, whether they need to go out of town for work, a family vacation, or an emergency. We are here to be your home away from home.

Child Care
Day Care & Preschool
St. Paul’s offers a full-service child care and preschool program at our Bankers Hill Community Care Center for children ages eight weeks to five years. St. Paul’s teachers and staff ensure our daycare program prepares children for kindergarten through the process of learning and discovery.

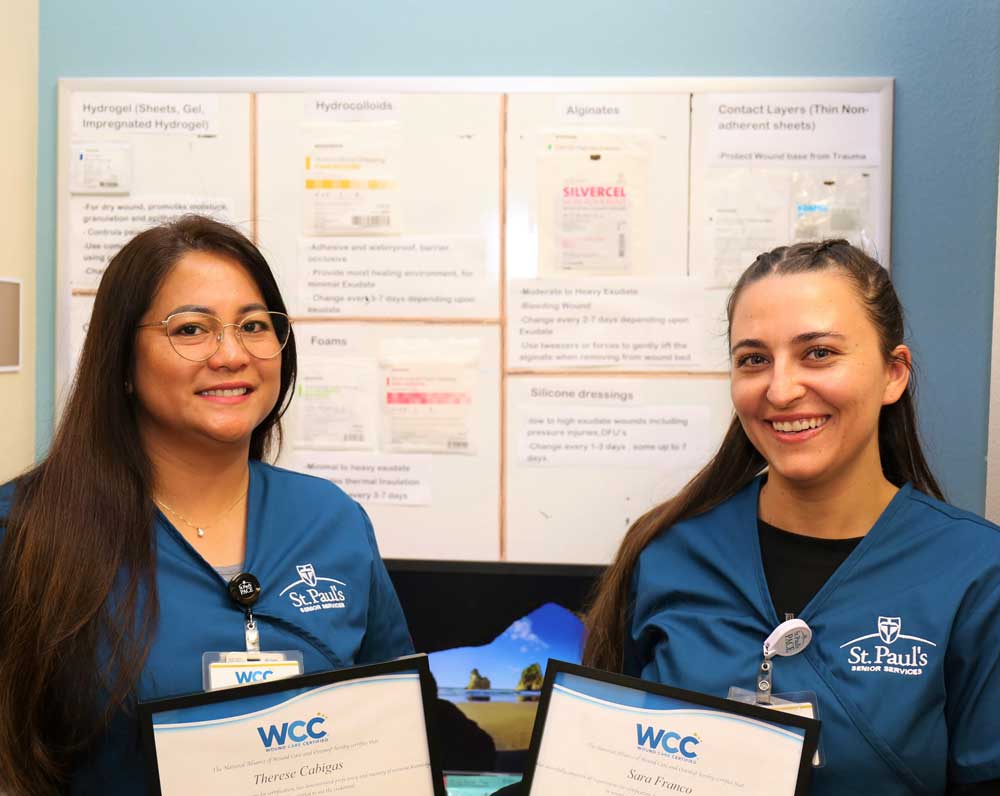
St. Paul's PACE
Managed Medical Care
St. Paul’s Program of All-Inclusive Care for the Elderly (PACE) provides wrap-around care services for San Diego’s frailest seniors. With four medical clinics in San Diego, St. Paul’s PACE provides free medical care, transportation, social work, nutrition, home care, day center activities, and more to those who are on or eligible for Medi-Cal.
Residential Communities and Programs
Located in central areas, St. Paul’s premium retirement communities are each unique to the resident they serve and the neighborhood they’re a part of.
From Chula Vista to Bankers Hill, our three senior living communities each offer an array of amenities, services, and programs for seniors to maintain active and purposeful lifestyles.
Explore St. Paul’s Communities